Altered sensorium
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence
based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box are welcome
CASE DETAILS
HISTORY:
A 42 yr old male, farmer by occupation, was brought to the casualty with chief complaints of altered sensorium, vomitings and fever since 2 days and was unresponsive since 2 days.
On evaluation, his GCS was E1V1M4.
HOPI:
Patient presented with complaints of 2 episodes of vomitings, 2 days back, with food as it's contents, and sudden in onset (?PROJECTILE).
The episode was preceded by hiccoughs.
Following the episode, he had frothing and spasm of neck muscles (?TONIC POSTURE), and loss of consciousness.
Vomitings were associated with fever with chills and rigors.
No history of pain abdomen, loose stools, cold cough.
He apparently lost his speech.
PAST HISTORY:
Patient had similar complaints in the past, with nearly 8-10 episodes of vomitings at night, 1 month back, sudden in onset, non bilious, non projectile, non blood tinged, contents being food,
History of alcohol consumption prior to vomiting.(10/9/2021)
Treated by RMP, with I.V fluids, condition improved.
Symptoms recurred 2 days later( 12/9/21)
Followed by involuntary movements of the upper and lower limbs associated with frothing and loss of consciousness. (?GTCS)
(FIRST EVER SEIZURE EPISODE) on 12/9/21 night.
Post ictal confusion present.
Associated with fever ,chills and rigors.
He was taken to a private hospital, managed conservatively and he IMPROVED and gained consciousness after 2 days. (Treated as DYSELECTROLYTEMIA.)
No history of loss of speech.
History of UTI during hospital admission which was resolved.
Started deteriorating 3-4 days later (18/9/2021)..
Adviced to get an MRI, therefore shifted to our hospital on 18/9/2021, 4pm.
Patient also had back pain 1yr back, following a fall at his workplace under the influence of alcohol, due to which he was asked to stop consumption of alcohol because of jaundice.
Patient stopped working because of generalized weakness since 1 year.
History of ALCOHOL WITHDRAWAL SYMPTOMS. (Tremors and cravings)
No known history of DM, HTN, asthma, epilepsy, TB.
His past history can be more extensively viewed here:
PERSONAL HISTORY:
Diet: Mixed
Appetite: Decreased
Sleep: Decreased
Bowel and bladder movements regular.
Addictions: WHISKEY, 150, ONCE WEEKLY, since 15 years
Stopped 1 year ago, (Apparantly)
PAN (ZARDA) chewing everyday. Since 15 years.
No history of smoking.
Allergies:. No known food or drug allergies.
GENERAL EXAMINATION:
Patient was drowsy, but arousable.
Afebrile,
BP: 100/60 mm Hg
PR: 92 bpm
RR: 20 cpm
SpO²: 99% on RA
Pallor: absent
Icterus: absent
Clubbing: absent
Cyanosis: absent
Lymphadenopathy: absent
Edema: absent
Respiratory system: Bilateral air entry +
Cardiovascular system: S1 S2 heard.
Per abdomen: soft, non tender, no scars or sinuses, bowel sounds present.
CNS examination:
He is drowsy, with loss of speech, GCS E1V1M4.
Motor power:. UL. LL
R 3/5 3/5
L 3/5 3/5
Tone increased in all 4 limbs.
Reflexes:.
B T S A K P
R. 2+ 2+ 2+ 2+ 2+ Extensor
L. 2+ 2+ 2+ 2+ 2+ Extensor
Signs of meningeal irritation:
KERNIG'S POSITIVE
Doll's eye sign: PRESENT
INVESTIGATIONS:
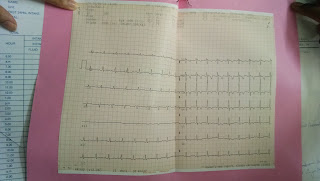
ECG:
Rate: 100-110 bpm
Rhythm: Regular sinus rhythm
Axis: Normal axis
T wave inversions present in precordial leads
MRI BRAIN:
No abnormality detected in brain.
SERUM ELECTROLYTES:
Past values:
Serum Chloride: 90
Sodium: 132
Potassium: 4.1
Patient was discharged on 26/9/21
Re-admission:
On 1/10/21:
Serum chloride: 182
Sodium: 142
Potassium: 16.4
Serum chloride: 94
Sodium: 125
Potassium: 4.8
On 3/10/21:
Serum chloride: 98
Sodium: 132
Potassium: 4.2
On 4/10/21:
Serum chloride: 98
Sodium: 131
Potassium: 4.2
Ophthalmology referral:
No signs of raised ICT present after complete evaluation
Past psychiatry referral:
Alcohol abstinence from 1 year
Lapse on 10/9/21, consumed 12 units of alcohol.
Based on this, it HIGHLY UNLIKELY FOR THE SEIZURES TO BE DUE TO ALCOHOL WITHDRAWAL.
Rule out neurological causes.
Present ophthalmology, psychiatry and surgery referral:
PROVISIONAL DIAGNOSIS:
Euvolemic hypoosmolar Hyponatremia,
(?SIADH)
? Bacterial/ TB meningitis
TREATMENT:
SOAP NOTES DAY 3
Subjective-
No fever spikes
Objective
On examination :
Pt is c/c/c
Oriented to t/p/p
patient is able to talk and started oral feed
No signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy
Vitals:
TEMP 98.2F
PR: 90 bpm, regular
RR: 15cpm
BP: 110/80 mmHg
SPO2:
AT ROOM AIR-99%
GRBS:101mg/dl
Systemic examination :
CVS:S1,S2 heard
Apex beat:5th ICS
Resp:
BAE+(vesicular breath sounds)
Nvbs heard
Position of trachea- central
P/A: soft, tenderness absent, bowel sounds heard
Cns: No focal deficit
HMF+
SPEECH-NORMAL
MEMORY-intact
No meningeal signs
Pupils-NS RL
MOTOR
Power-(4/5 4/5)
Tone-(Normal in all 4 limbs)
Reflexes-
B T S A K P
R 2+ + - + + flexion
L 2+ + - + + flexion
Assessment-
Altered sensorium secondary to ? Hyponatremia(resolved)
with alcohol withdrawal seizure(resolved)
With pyrexia secondary to UTI
No fever spikes
Plan of care-
head end elevation
inj levipil 800mg in bd
inj optineuron 1amp
inj monocef 2 lgm iv
inj Vancomycin 500mg in 200ml NS
Inj Neomol 1gm iv sos
tab pcm 650mg
tab tolvapt 15mg
double strength Ors
monitoring vitals 4th bourly
.Monitor vitals-4rth hourly
I/O charting












Comments
Post a Comment