Fever and Sob
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box are welcome
HISTORY:
Date of admission: 18/10/2021
Patient came with the chief complaints of:
1. SOB since 3 hrs, grade 4
2. Fever since 6 days.
HISTORY OF PRESENT ILLNESS:
Patient was apparantly asymptomatic 1 week back, then he had a fall, no loss of consciousness, and sustained a 2×1cm abrasion on his scalp.
Following this he developed low fever, since 6 days, which is intermittent, not relieved on taking medications, not associated with chills and rigors.
Shortness of breath since 3 hrs on DOA, grade 4.
PAST HISTORY:
He had a history of repeated falls 1 year back , for which he went to the government hospital.
Initially the patient was told that he had low blood pressure, then after 5 months , he was diagnosed with hypertension and started taking medications.
He had a history of pedal edema and shortness of breath 1 year back for which he came to KIMS . He was diagnosed with Renal Failure and was on conservative treatment for 4 months, then he stopped taking medication and is only on Tab NODOSIS till now.
Patient had the history of fall 1 week back , no history of loss of consciousness, had a small abrasion on the head.
Patient had constipation for 2 days , took DULCOLAX tablets, had loose stools (3 episodes)
The patient is a known case of Hypertension, is on Tab AMLODIPINE 5mg.
PERSONAL HISTORY:
Diet: vegetarian diet since 6 years
Sleep: adequate
Bladder movements: normal
Bowel: Constipation
Addictions: He used to smoke 18 beedis/day , smoked for 30 years. After he was diagnosed with Tuberculosis (took treatment for 2 years) , he stopped smoking.
He was an alcoholic , took 90ml/day and stopped 1 year back, now takes occasionally during social gatherings.
Allergies: No known allergies.
GENERAL EXAMINATION:
Vitals on admission:
Temperature - 98.4 F
Pulse rate - 92bpm
Respiratory rate- 22/min
Blood pressure- 150/70mm Hg
SpO2 at room air- 90%
GRBS - 120mg/dl
SYSTEMIC EXAMINATION:
CVS - S1 S2 present, no murmurs
RS - pleuritic rub heard
P/A -
No tenderness
No palpable mass
CNS - NAD
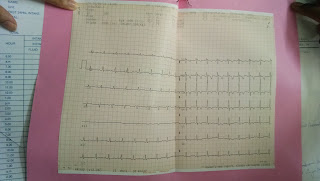
INVESTIGATIONS :
Rapid Antigen Test for Covid - negative
ABG at 3 AM on 19/10/21:
pH - 7.44
pCO2 - 38.2
HCO3 - 25
pO2 - 57.2
Hemogram:
Hb- 12.7 g/dl
TLC - 22,400
N/L/E - 63/32/02
PLC - 2.45 lakhs
RFT :
Urea - 39
Creatinine- 1.2
Na - 132
K - 3.9
Cl- 92
LFT :
TB - 1.3
DB - 0.5
AST - 28
ALT - 12
ALP - 136
TP - 6
A/G - 0.7
RBS - 118mg/dl


Comments
Post a Comment